ROI grants advance a new era of radiotherapy
The Radiation Oncology Institute (ROI) has recently selected six exceptional research teams to receive grants that will support innovation in the delivery of radiation therapy (RT) to improve outcomes for patients with cancer. The awards are the result of the “New Era of Radiotherapy” request for proposals that ROI issued last fall to stimulate research on emerging challenges and cutting-edge methods that are transforming the practice of radiation oncology. This year’s ROI grantees will investigate a variety of timely topics through novel research that aims to help people with cancer live longer, healthier lives.
Climate Change and Cancer Care
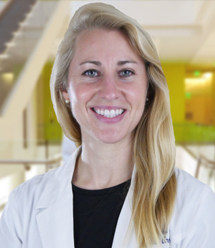
Climate-driven disasters can disrupt cancer patient care, specifically radiation therapy, which can have adverse effects on survival rates. The increasing frequency and intensity of climate-related weather events contribute to this concern.
Katie Lichter, MD, MPH, will investigate how wildfire events impact the provision of radiation therapy. Dr. Lichter’s team will survey California-based radiation oncologists to assess their perceptions and preparedness for such events. Additionally, they will analyze care disruptions for patients receiving radiotherapy during such events and study whether wildfire exposure affects survival in lung, cervical or head and neck cancer patients. Dr. Lichter is a PGY-3 resident in the Department of Radiation Oncology at the University of California, San Francisco.
GRID Therapy as Curative Treatment

In GRID therapy, a type of spatially fractionated radiation therapy, patients are treated with a very high dose of radiation to a small area of their tumor while adjacent areas get a low dose. The technique could potentiate the effects of radiation while minimizing toxicity.
Ted K. Yanagihara, MD, PhD, will conduct a pilot study to treat patients with extremity soft tissue sarcoma with a single dose of GRID therapy prior to standard pre-operative radiotherapy and surgery to remove the tumor. Dr. Yanagihara’s team will test whether GRID is safe and effective and will analyze post-GRID biopsies to look for evidence that the immune system was activated within the areas of sarcoma that received a low dose. Dr. Yanagihara is an assistant professor in the Department of Radiation Oncology at the University of North Carolina at Chapel Hill.
Unlocking the Potential of FLASH Radiotherapy
FLASH radiotherapy delivers an ultra-high dose more than 300 times faster than conventional radiotherapy. FLASH RT has been shown to reduce toxic side effects of radiation in healthy tissues and could support much shorter treatment times and the delivery of higher doses of radiation for patients who need it.

Nicholas Colangelo, MD, PhD, will investigate whether a class of drugs called superoxide dismutase (SOD) mimetics can enhance the effects of FLASH RT in pancreatic cancer, which has one of the lowest rates of survival. Dr. Colangelo’s team will conduct preclinical research to show that FLASH RT and SOD mimetics work together to reduce toxicity, shrink tumors and improve survival. Dr. Colangelo is a PGY-3 resident in NYU Langone Health’s Department of Radiation Oncology participating in the Holman Pathway. He is also part of Perlmutter Cancer Center. ROI selected Dr. Colangelo as the winner of this year’s James D. Cox Research Award to support his groundbreaking research that has the potential to improve treatment for patients with pancreatic cancer.

Michael Goldstein, MD, PhD, will develop a FLASH RT regimen for lung cancer that consists of multiple treatments to test whether this type of radiation delivery retains its protective effect on nearby healthy tissues. Most FLASH RT studies to date have used a single high dose of radiation, whereas conventional RT that is used in clinic for treatment of lung cancer patients is fractionated and administered in many small doses over multiple weeks. Dr. Goldstein’s team will use a cutting-edge platform to conduct preclinical studies on fractionated FLASH RT that will help establish whether it will be safe and effective to test in lung cancer patients. Dr. Goldstein is an assistant professor in the Department of Radiation Oncology at the Johns Hopkins University School of Medicine.

Joseph Harms, PhD, will build and test a new detection system to measure the dose and how fast the dose is delivered (dose rate) for FLASH RT. A key step in safely delivering radiation therapy to patients is verifying that the delivered dose matches the planned dose. Currently, there is no accepted way to verify dose rate from FLASH RT treatment plans, and many of the commonly used radiation detectors do not function at the very high dose rates of FLASH. Dr. Harms’s team will develop a radiation detector that uses an ultra-fast camera and will allow for real-time measurement of FLASH beams to ensure that treatments are delivered to patients as intended. Dr. Harms is an assistant professor of medical physics in the Department of Radiation Oncology at the University of Alabama at Birmingham.

Michael Pennock, MD, MBiot, will compare three methods of delivering proton therapy for head and neck cancer, including a new FLASH modality developed by his team. Many proton FLASH studies use transmission proton FLASH, where beams traversing the patient’s normal tissues have been necessary to generate FLASH dose rates. Modalities that maintain FLASH dose rate while minimizing the dose to normal tissues would be beneficial. In prior research, Dr. Pennock’s team has shown that their novel method of proton pencil-beam scanning Bragg peak FLASH (PBS-BPF) can eliminate the exit dose beyond the tumor target, maintain FLASH dose rates and potentially reduce side effects caused by damage to healthy tissues. Through preclinical and translational research on PBS-BPF, transmission proton FLASH therapy, and conventional proton therapy, Dr. Pennock’s team aims to determine which treatment best minimizes damage leading to side effects that jeopardize eating and speaking for patients with head and neck cancer. Dr. Pennock is a PGY-4 resident at Montefiore Einstein Cancer Center.
These innovative, award-winning teams are working toward discoveries that will advance the field of radiation oncology and enhance care for patients with cancer. Follow ROI on Twitter, Facebook, and LinkedIn for the latest news on these new projects and all of the research made possible through the generosity of ROI donors.